6 min read
Increase Satisfaction and Reimbursement by Knowing What Patients Want
By: Lori Zindl on Dec 11, 2019 10:52:24 AM
If you ever doubted that interactions between patients and your registration and billing staff are important to reimbursement, consider how the Affordable Care Act ties reimbursement to patient satisfaction.
Here’s how:
The Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) is one of the US government’s most important tools to provide meaningful comparisons among hospitals. Patient feedback will account for approximately one-third of a provider’s Medicare and Medicaid reimbursement scores, and research shows that reaction is usually based on the patient’s most recent interaction with the provider, which typically is billing and collections.
The way you communicate with them during these processes may have a big impact on reimbursement.
Although healthcare providers have been conducting surveys on patient satisfaction for their own internal use, until HCAHPS there was no national standard that allowed valid comparisons to be made across hospitals locally, regionally and nationally.
With patient satisfaction being so closely tied to reimbursement and financial rewards, healthcare organizations have been motivated to improve the patient experience.
Offering Payment Options
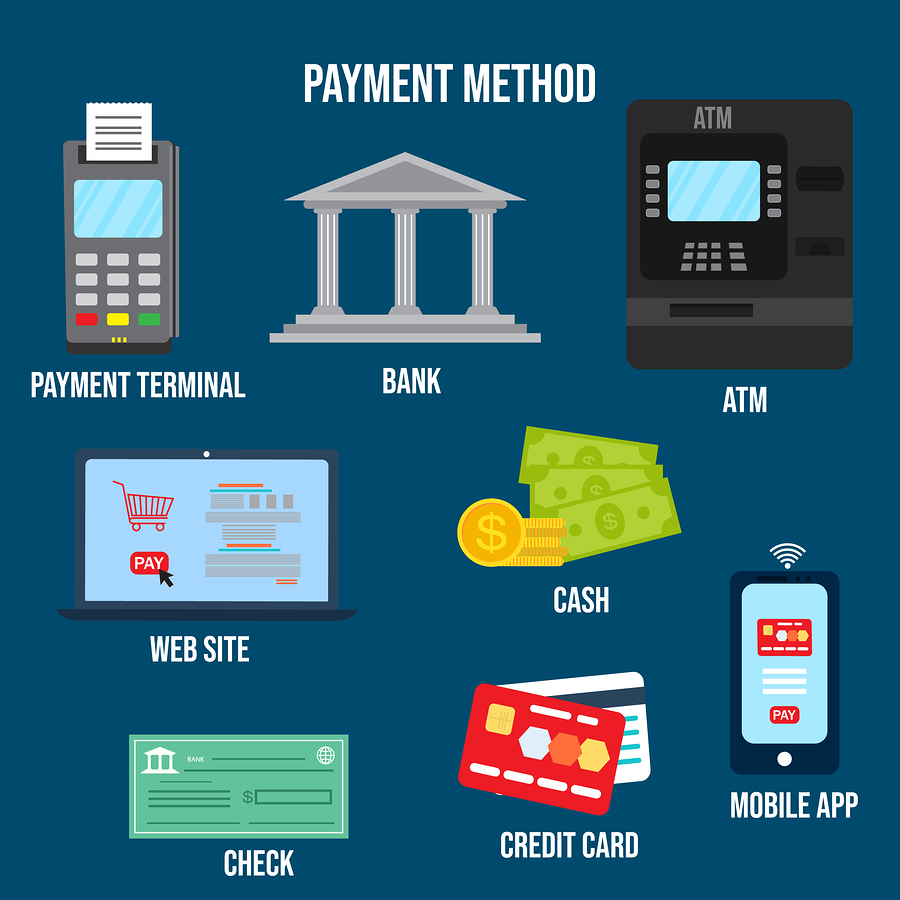
One way to improve your connection with patients and enhance the patient experience is to provide multiple options for them to contact you and to make payment.
Unless you are in a specialty practice, your patients are likely a diverse group that will prefer different ways of connecting with you. And, while HCAHPS affects Medicare reimbursement, you also should consider the preferences of patients in other age groups as well.
For example, research shows the Millennial Generation (born between 1982 and 2004) prefers easy access to their providers, whether it is ensuring information is online and easy to find, making an organization’s patient portal relevant while avoiding phone calls and voicemails. Because they were raised on the convenience of the 24/7 news and information cycle, many Millennials prefer communicating via the web, not by traditional telephone calls. And, they prefer to connect to the web via their smartphones.
Another survey conducted by Inlet, a new technology platform that enables companies to securely deliver digital documents across multiple online consumer destinations, found that younger patients are shunning traditional payment methods, with less than one of four paying their basic bills by mail.
Patients of all ages have become more computer literate. A study conducted by Pew Charitable Trusts revealed that Gen Xers (born between 1965 and 1981) own smartphones but are “heavy users” of credit cards and may be less inclined to make mobile payments, but still want those options.
At the same time, older patients are getting into using technology, too. Federal Reserve data shows that less than 13 percent of Baby Boomers still prefer to pay by sending a check through the mail or pay with cash.
Healthcare providers may already offer a variety of contact methods that successfully cover many types of patient/provider interactions, such as the following:
-
Integrated Call Center. Patients still have occasions when they want or need to speak to a human being. It might be because of billing or payment issues, but it might also be an elderly or financially needy patient who has other types of questions about appointments and other issues.
-
Online Payment. It isn’t the same as talking to a human in a call center, but online web portals are available 24 hours a day, and they can provide moderately tech-savvy patients with the same guidance. A user-friendly portal will offer the patient a variety of payment options, use clear language, publish relevant documents such as patient statements, and prompt the patient to pull out their credit/debit/HSA card and make a payment.
-
Voice Response. Patients don’t always have time during normal business hours to spend on hold for a call center rep, so providing them with the option to make a payment at night, early in the morning, or without wait can boost reimbursement significantly.
It seems that regardless of age, offering a variety of payment options is an important aspect of your billing and collection program, and it may improve recovery as it affects patient satisfaction.
Convenience is important!
Be Aware of Privacy
If you are using email or text communication as a form of communication with patients – especially physicians and patients – be aware of required safeguards to keep electronic protected healthcare information (e-PHI) secure throughout such communication.
The HIPAA (Health Insurance Portability and Accountability Act) Privacy Rule allows and sometimes even requires hospitals and other covered entities to communicate with their patients via email or text if they request it. With this requirement, however, also comes important protections that must be adhered to when sending e-PHI to patients.
When sending emails, for example, healthcare providers must be sure to verify the email address for accuracy before sending or send a message to the patient verifying the email address before sending the email that contains e-PHI.
Providers are also advised to limit the amount and type of information disclosed through an unencrypted e-mail, and in doing so should document why it would not be “reasonable and appropriate” to encrypt the included data. The patient also must be warned if a connection that is not secure or if the information in the message is not encrypted. In cases when more information is to be disclosed, the covered entity or business associate must encrypt the e-PHI in the email as reasonable and appropriate.
At the same time, these rules don’t apply to emails and texts sent by patients.
A patient might send health information to a healthcare provider using email or texting that is not secure, because it is assumed that in this case, the communication is acceptable to the patient because, after all, they sent it.

Revenue Cycle Matters Tip: We suggest using every opportunity that presents itself to educate patients and staff on the importance of security when it comes to PHI. We always advocate for using the minimum information necessary when communicating on patient accounts. In many cases, staff can use non-identifiable reference numbers like claim ID to communicate on issues and limit the risk of exposing PHI.
Denials
Further down the line, communication with patients – or lack thereof – can be tied to claim denials. Around a third of all denied claims are associated with inaccurate patient information. According to a survey from Black Book Research, these denials cost the average hospital $1.5 million and the U.S. healthcare system over $6 billion annually.
One of the top billing errors named by nearly all surveys for causing claim denials is missing or incorrect information. A minor error such as a wrong name, an incorrect middle initial, or a wrong address can cause a claim to be denied by a payer, which can lead to a negative patient experience and bring down healthcare provider survey responses.
Another common denial that can have a negative impact on patient experience is medical necessity. Imagine being a patient, who receives a bill for a service deemed not medically necessary by their insurance.
Would you provide positive feedback on the next survey you received from that provider?
Denials also lead to delays in claim processing, which means a patient may not receive their bill until several months after their visit. No one wants to be billed for a service they received months prior, they might have even forgotten about it, so for any denials you do receive - be sure to work quickly to resolve them!
It’s critical that the patient access team receives denial education, so they understand the impact their actions have on both the organization’s bottom-line and on the patient experience.
Most revenue cycle teams have analytics capable of identifying the origin of denials. Analytics and reporting tools can be a great way to share real-world examples, provide constructive feedback and drive home the importance that of the registration process.
Why Revenue Cycle Matters to you?
Understanding which communication method your patients prefer is key to letting patients know that you care about what they want, and that you value them and their business enough to tailor your payment processes to their preferences.
We hope this information is valuable to you as you look for new ways to increase the patient experience. If your organization is limited in their abilities to perform root cause analysis on denials, consider getting in touch with one of our claim experts to schedule a demo of efficientC.
They will be happy to show you how our reporting and edits support better billing practices and a revenue cycle that increases collections.
Related Posts
12 Things Keeping Hospital CFOs Awake at Night
Is the pressure to simultaneously control costs and improve care quality making you toss and turn...
Is Your Business Office Leaving Money on the Table?
Staying on top of the healthcare needs in your rural community depends on the resilience of your ...
Protecting PHI on Mobile Devices
The convenience of mobile devices has revolutionized healthcare. Improvements in efficiency and...