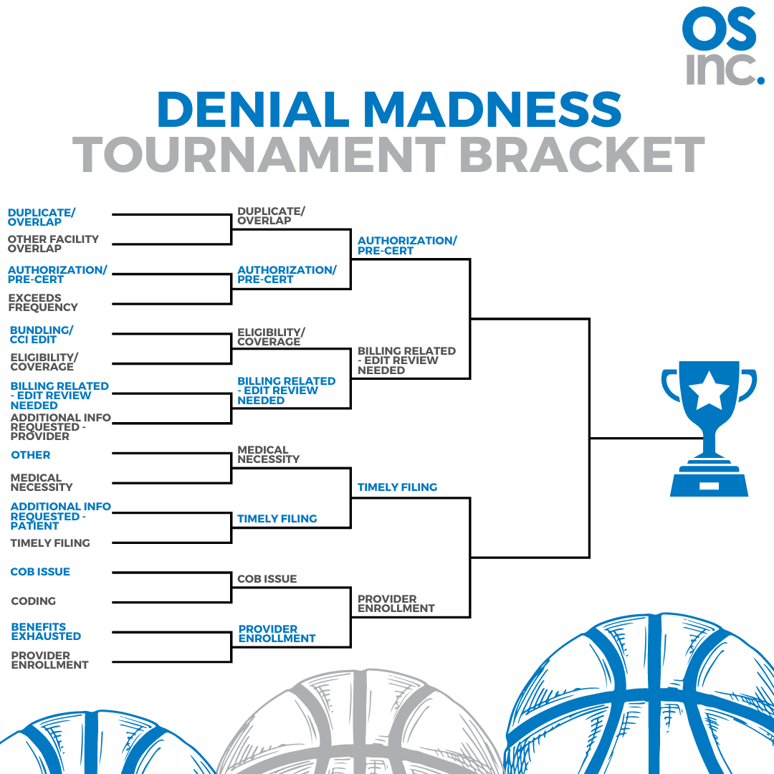
Well, we’re down to the last four denials (just like that other tournament). If you haven’t been following along you may want to catch up by reading our prior blog post. We discussed why we decided to move the eight denials forward as more preventable from our original sixteen.
A lot of the same logic applies as we move from eight to four. Denials that have less variables are the ones we know we can better prevent. Now for our disclaimer: these selections are general guidelines and there are always exceptions that may be unique to any given organization regarding preventable denials.
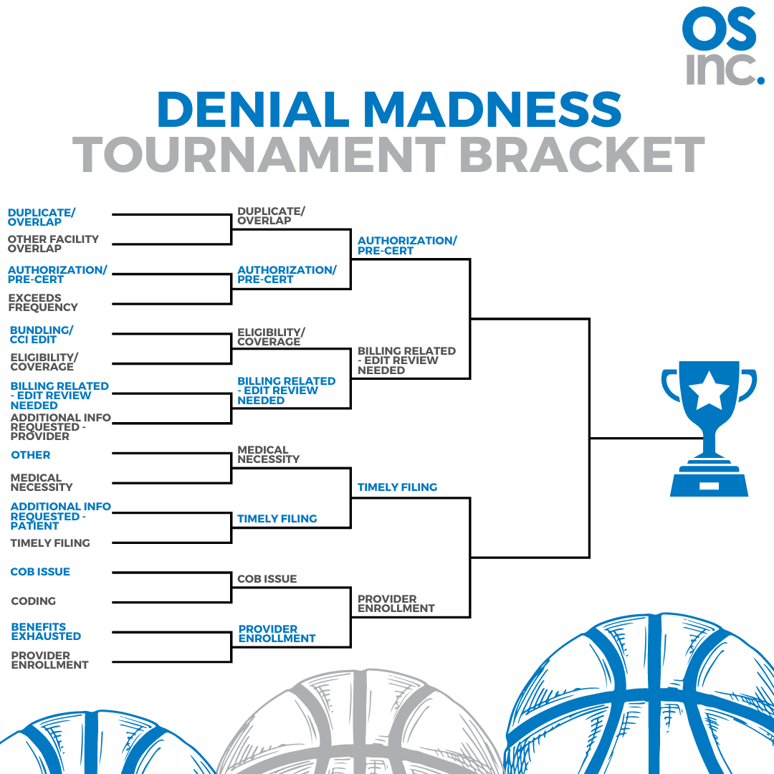
Bracket One: Duplicate and Overlap Denials vs Authorization and Pre-certification Denials
We know that all payers have a listing of which services require an authorization. If edits are set up appropriately, these claims can be stopped and worked before they go out the door. While we can set up edits with Duplicate and Overlap denials, the variety of denials is larger and not always known. When we know the rules that’s where we will always land. Winner: Authorization and Pre-certification Denials.
Bracket Two: Eligibility and Coverage Issues vs Billing Related – Edit Review Needed Denials
Tools do exist for eligibility and insurance coverage discovery, but not every organization has these tools. Even if you have them, it’s not a perfect science. With OS inc’s technology platform, it is a perfect science for the Billing Related – Edit Review Needed (a denial category unique to our platform). We know that every denial identified in this category can be prevented with an edit. If you’d like to hear more about our platform and see how we do it, let us know. Winner: Billing Related – Edit Review Needed Denials.
Bracket Three: Medical Necessity vs Timely Filing Denials
We ALWAYS know the timely filing limit. So we always know when these claims need to be worked to prevent them from being denied. Medical necessity denials can often have a payer specific rule that is not known. Medical necessity is one of those where unknown payer rule changes can really have a negative impact. Winner: Timely Filing.
Bracket Four: Coordination of Benefits (COB) vs Provider Enrollment Denials
Every organization knows their providers and every organization should know if they are credentialed. If a provider is not credentialed with a payer, these claims should be put on hold. Coordination of benefit denial prevention relies on insurance discovery tools. These tools are generally reliable, but ultimately out of your control. Winner: Provider Enrollment.
We are getting to the end of our Denial Madness Bracket Tournament. Thanks for following along so far. We will have one more update to wrap things up. Our goal during this exercise is to have a little fun but also share our denial prevention philosophy. Every claim we prevent from denying saves time and money. We are always focused on getting the highest First Pass Yield Rate on our claims as possible. If you’d like to discuss any of our preventable denial selections or if we can be of any assistance, don’t hesitate to reach out to us.